Pregnancy with an Abnormally Shaped Uterus
This article was medically fact-checked by Consultant Obstetrician and Gynaecologist Dr. Shree Datta.
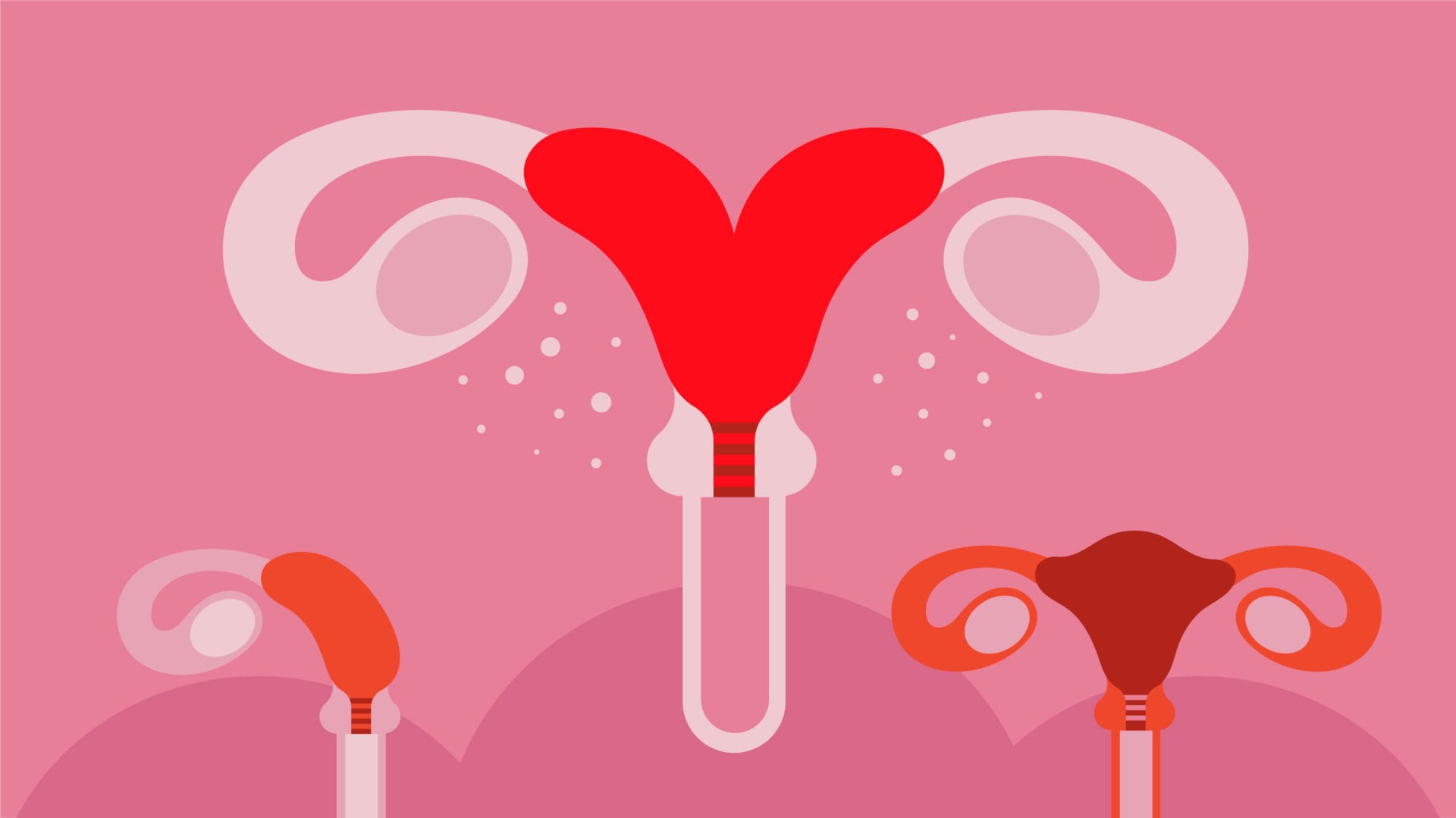
Most of us are familiar with the standard “pear-shaped” uterus, what you may not realize is that like humans, uteruses can also vary in shape and size.
Uterine abnormalities can change the size, shape, and/or structure of the organ. The estimated rates of congenital uterine anomalies, CUAs, are 5.5% in an unselected population, 8.0% in infertile women, 13.3% in those with a history of miscarriage and 24.5% in those with miscarriage and infertility.
For many, this could go undetectable their whole lives. Most people are totally unaware of any uterine abnormality until they go for surgery, some sort of scan- like an ultrasound, attempt to conceive, or become pregnant.
Let’s take a look at what kind of uterine abnormalities are out there, and how that may affect someone’s reproductive journey.
Uterus Didelphys: Also known as a double uterus.
People with a double uterus make up a small percentage of those with uterine abnormalities, affecting an estimated one in 2,000 women.
This occurs in utero when the two tubes that normally fuse into one uterus remain separate. They may each have their own cervix, or share one. In rarer cases, a person with this condition may even have two vaginas- the canal, not the opening.
A double uterus may cause someone to have a heavier flow during their period, without realizing why. In painful and rare cases, one of the uteruses may not have a vaginal opening, causing it to fill with blood during the period, and not be able to drain.
It’s entirely possible for someone with a double uterus to carry a baby to term with no issues, however, there are definite risks. It’s somewhat common for those with a double uterus to have recurrent miscarriages. When they go in for scanning to see why this keeps happening, that’s when they learn about their condition.
If someone with a double uterus does conceive, they have the possibility of abnormal fetal presentation, an increased chance of delivery by cesarean section, intrauterine fetal growth restriction, and low birth weight less than 2500 g (5.5 lbs), as well a heightened chance of perinatal mortality. There is also an increased risk of premature birth, before 37 weeks gestation, by up to forty-five percent.
Although it’s usually not medically necessary, a double uterus can typically be surgically corrected. This is usually only done in the case of repeat miscarriages.
Bicornuate Uterus: This type of uterus is often called a heart-shaped uterus. It forms in the womb similarly to a double uterus, however, it doesn’t fully split all the way, and instead creates one uterus with two “horn-like” features at the top, and a septum deviating them in the middle, creating a heart shape.
People with a heart-shaped uterus typically have no issues with conception or early pregnancy, but problems could arise later on as the baby has less room to grow and move around.
Without the extra wiggle room, the baby could potentially experience IUGR, or Intrauterine Growth Restriction, which could potentially lead to other problems in pregnancy. A heart-shaped uterus does come with an increased risk of miscarriage and preterm birth.
Another common result of pregnancy with a heart-shaped uterus is a baby with breech presentation. This is when instead of their head being down, their bottom or feet are.
Breech vaginal deliveries are entirely possible and safe, however many providers and hospitals in different areas will have stricter rules around breech birth.
It’s also common for healthcare providers do not have proper training for how to assist breech births, which leads to a higher likelihood of induction or c-section.
This all may depend on where the uterus divides, how far down the septum goes, and how well the woman’s uterus grows with pregnancy.
If you have a heart-shaped uterus and are hoping to have a vaginal delivery, it’s important to find a provider in your area who has experience with breech deliveries. This could make the difference between having a c-section, and not having one.
Like a double uterus, heart-shaped ones can be repaired with surgery, although many people have normal pregnancies and vaginal deliveries with no issues!
T-Shaped Uterus: It looks like how it sounds, these uteruses are in the shape of the letter T. While this is pretty rare in the average population, there was a medication, utero diethylstilbestrol (DES), prescribed to pregnant women in France from the years 1948-1971, when it was banned, that greatly increased the prevalence of T-shaped uteruses.
While this medication was thought to prevent pregnancy loss, the exposure of this synthetic estrogen in utero, caused many women to be born with a T-shaped uterus.
Ironically, this can have adverse effects on their ability to bring babies to full term, although not necessarily on their ability to conceive. In a study focused on women exposed to DES in utero, researchers found these women to have a statistically significant increased risk of ectopic pregnancy, miscarriage, and preterm delivery.
Like with the other abnormalities we mentioned, some women are able to have normal, healthy pregnancies with a T-shaped uterus, while others choose to have it corrected with a surgical procedure called a metroplasty. For some women, this procedure can greatly increase their ability to have a full-term live birth.
You are Woman
These three aren’t the only kind of uterine abnormalities out there. Some are congenital, ones that people are born with, while others like a tipped uterus, can occur as a result of pregnancy, endometriosis, or fibroids.
While none of this information should be taken as medical advice, it may offer you some clarity, and hopefully, support in your reproductive journey. The shape of your uterus, and the direction of your pregnancy journey does not make you any less of a woman. Our differences give us character, and make the world go ‘round!
Facts checked by:
Dr. Shree Datta
Dr. Shree Datta is a Consultant Obstetrician and Gynaecologist in London, specialising in women’s health including all menstrual problems such as fibroids and endometriosis. Dr. Shree is a keen advocate for patient choice, having written numerous articles and books to promote patient and clinician information. Her vision resonates with INTIMINA, with the common goals of demystifying periods and delivering the best possible care to her patients
Written by:

Natasha (she/her) is a full-spectrum doula and health+wellness copywriter. Her work focuses on deconstructing the shame, stigma, and barriers people carry around birth, sex, health, and beyond, to help people navigate through their lives with more education and empowerment. You can connect with Natasha on IG @natasha.s.weiss.




Diabetes is a condition that causes high levels of glucose in your blood. Glucose is a sugar that is your body’s main source of energy. Health problems can occur when your glucose levels are too high. When diabetes starts during pregnancy it is called gestational diabetes and it is of special concern.
If your blood pressure increases slightly during your pregnancy, bed rest at home or in the hospital may help keep preeclampsia from developing. If preeclampsia does develop, the only real treatment is to have the baby because continuing the pregnancy can result in damage to your organs, including your kidneys, liver, brain, heart, and eyes. Although preeclampsia typically lasts for up to two weeks after delivery, it always goes away after a pregnancy.
I am a daughter of a woman who was made to take DES during her pregnancy with me, as well as while pregnant with my younger brother (births in 1957 and 1959). I’ve met quite a few other women born in the USA, whose mothers took DES. I notice that, in the section on T-shaped uterus, you specify only that DES was prescribed to pregnant women in France. This seems very misleading to me, as it was certainly fairly widely prescribed to pregnant women in the USA. I don’t know about other countries. It seems people coming to this site for information might read that and think, “Oh, then my mother wouldn’t have taken DES, because she wasn’t in France.”
In fact, my parents moved back to the USA from France when my mother became pregnant again, after having had one healthy, full-term baby, and then a very premature one, who did not survive. They figured that, at that time (1954) medical care and technology around pregnancy and birth would be more advanced in the US. In fact, she unexpectedly gave birth to a very premature baby quite soon after their ship landed. (According to my mother, this baby was born exactly one year after the earlier premature one, exactly the same amount of time premature; she did like to embellish a story, so I don’t know how accurate that was.) This baby did manage to survive, spending many of her first weeks in an incubator. It was very touch and go, according to the doctors, and was a traumatic, devastatingly expensive ordeal. Therefore, when my mother became pregnant again, in 1957, she expressed her worries about possible prematurity, and her doctor prescribed DES, telling her to take one pill every day, “like a vitamin.”
I have been told that I have an unusually shaped/oriented uterus, unlike my older sisters. Also unlike them I have osteopenia, despite having had far more, and more intensive, weight-bearing exercise for much of my life, due to profession. I never gave birth to children, and, since learning about my DES history, have had doubts that I could have had a successful pregnancy.
All more than you needed to know, but I think you should change that wording, to reflect the actual locations where DES was prescribed.