What in the World is Vulvodynia?
Vulvodynia. Upon hearing this, did you think of a dinosaur-shaped like a vulva? You’re not the only one.
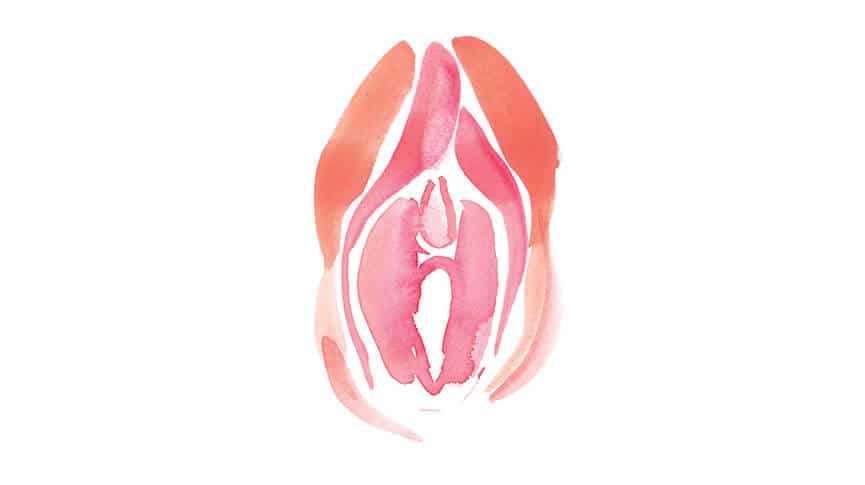
While this imagery is hilarious to think about, the reality of vulvodynia is not as funny. Vulvodynia is a broad stroke term for pain in the vulva lasting three or more months, without a known cause.
Depending on the person, this pain tends to increase with penetration and excessive friction in the vulvar area. This can make everyday activities like sex, sitting, and living incredibly painful.
While it usually affects the vulvar opening, it can also occur in the clitoris, which is known as clitorodynia.
Ouch. The vagina dinosaur is starting to sound more and more appealing.
What’s The Deal?
What makes vulvodynia so elusive, is that it can manifest as a myriad of different symptoms, and can be difficult to pin down. Burning, irritation, itchiness, stinging, swelling, soreness, and throbbing are just a few of the symptoms someone with vulvodynia may experience.
Along with the inherent shame we often carry about our reproductive organs, it can keep people from opening up and disclosing early on any pain they may be experiencing.
Genetic Predisposition
Certain genetic disorders can cause vulvodynia to develop. In some cases it may be the first symptom that’s indicative of a more serious problem.
People with vulvodynia are up to three times more likely to have suffer from a comorbid chronic pain condition like fibromyalgia, irritable bowel syndrome, and interstitial cystitis.
In these people, the presence of vulvodynia may indicate an underlying neurological condition as a result of Central Sensitization. A result of a hyperactive nervous system that registers normal sensations as painful.
Another comorbidity factor is people with multiple sclerosis. While scientists are not totally clear on how MS works, it is typically described as an autoimmune disorder affecting the nervous system- which can lead to chronic pain. Vulvodynia occurs in people with MS for presumably the same reasons as with other underlying disorders- the effect on the nervous system.
Trauma and Childbirth
Other potential causes of vulvodynia can come from physical and emotional trauma, as well as childbirth. An injury to the area of the spinal cord that connects to the vagina can cause symptoms of pain in the vaginal area.
Vulvodynia associated with trauma does not necessarily mean a direct injury to the vulvar area. People with PTSD and depression disorders had a 50% higher prevalence of vulvodynia.
Think You Might Have Vulvodynia?
If you think you may have vulvodynia, it’s ok to ask for help. Go to your gynecologist or health care provider, and try to disclose all details that may help with your diagnosis and treatment.
Depending on the severity of your symptoms, the intensity of treatments and interventions may vary.
At Home Pain Management
- CBD used topically/and or ingested orally is a powerful tool for any sort of pain management. These compounds found in the cannabis plant offer pain relief, without mind altering effects. Its ability to act on the endocannabinoid receptors in the brain, may also help treat certain neurological disorders- like the ones associated with vulvodynia.
- Yoni Steam: In this practice which stems from various traditional systems of medicine, people squat or sit over steaming water infused with herbs. While the medicinal effects of the herbs can help relieve symptoms of vulvodynia, the steam itself helps to increase circulation in the pelvic area, which helps with blood flow.
- Beware of chemicals from laundry and body soaps, clothes, lubricants, and condoms, as these common irritants can throw off your delicate pH balance, disrupting the vaginal flora. Research suggests an increased amount of pain from vulvodynia in patients with abnormal vaginal flora levels.
- Icing: While this may not get to the root of the cause, it can provide some easy, quick pain relief, and decrease swelling.
Seeking Treatment
There are a number of modalities which have helped people in their healing from vulvodynia.
- Sexological Bodywork: A form of bodywork that focuses on the connection between our nervous systems and reproductive organs. Practitioners use a variety of techniques, including vaginal massage to help relieve pain and discomfort from disorders like vulvodynia.
- Botox: While this may seem extreme, botox is used in a variety of pain management disorders from migraines to vulvodynia, by helping relax the affected muscles, like those of the pelvic floor.
- Mental Health: Given the strong correlation between mental health disorders and vulvodynia, it makes sense that seeking mental health treatment, and practicing self care can help reduce symptoms of vulvodynia.
- Acupuncture: May help with pain management, as well as mental health-related factors. By stimulating deep parasympathetic nervous system responses, acupuncture helps relax the patient, and decrease symptoms of chronic pain.
- Gabapentin: A pharmaceutical drug used to treat seizures, has been shown to help increase sexual pleasure in people with vulvodynia.
No matter what the underlying cause is, your pain is valid, as are your reactions to it. Vulvodynia can be an emotional journey, and you deserve all the support in navigating it.

Natasha (she/her) is a full-spectrum doula and health+wellness copywriter. Her work focuses on deconstructing the shame, stigma, and barriers people carry around birth, sex, health, and beyond, to help people navigate through their lives with more education and empowerment. You can connect with Natasha on IG @natasha.s.weiss.



My Dr said not many professionals don’t know about this. But a Urogyno told me it could be Purdendal because I mentioned my feet burning. Then I’m trying PT. I’ll try whatever works. Help please